Review of Moseley/Hodges Conference Part Four
In this post I will conclude my review of Lorimer Moseley's talk. Here are links to parts one, two and three. Before getting started with part four, which mostly covers how nociceptive signals are modulated, I wanted to share a little phrase that Moseley repeated on numerous occasions.
"We are fearfully and wonderfully made."
He explained that he first heard this phrase from an elementary school science teacher. "Young man, we are fearfully and wonderfully made."
When he first heard it, he completely disagreed, but now he has obviously changed his mind. He used it repeatedly at the conference, usually right after explaining some particularly mind boggling result from his research.
I think it was his way of communicating his sense of excitement and privilege to study the nervous system, coupled with humbled awe and respect that we are only scratching the surface of the most complex thing in the known universe. We are fearfully and wonderfully made for sure.
I think it's a nice thing to have in mind when approaching the question of how to help someone in pain. So here's some more fearful and wonderful information from the conference.
Nociception: some language issues
Nociception is defined as activity of high threshold Adelta and C nerve endings, which are designed to detect mechanical, thermal, or chemical changes in the tissues. Many people refer to nociception as "pain signals", but Moseley does not approve.
To understand why, recall that nociception is only one of many inputs which contribute to the output of pain. Other inputs may be purely cognitive, such as believing that you have a "slipped disc." Would we consider the auditory information that delivers this (false) belief to be a "pain signal"? No. Then why call nociception a pain signal? If we do that, we place inappropriate focus on one particular input into the system, and deemphasize other inputs which might be just as important. For example, people tend to think of "psychosocial" issues as an afterthought if they are too intent on finding where the "pain signals" are coming from.
Which brings up another point that Lorimer made. Namely that he doesn't really like the term "biopsychosocial." The term implies a false trichotomy, as if psychological or social contributors to pain somehow lie outside the realm of biology. It's all "bio" really - psychosocial events only contribute to pain to the extent that they affect biology. But if we forget this, then there is the implication that pain of psychosocial origin is less real than pain which is "bio", and of course this is not accurate and also stigmatizing.
Personally I've always hated this term - it's too long, it sounds dumb, it's imprecise and confusing. I suppose it serves a useful purpose because everyone else uses it. Whatever!
Stages of nociception
The process of nociception proceeds through several stages. It is initiated at free nerve endings when they are triggered by changes in temperature, chemistry or mechanics. This is called primary nociception, and it sends a nerve impulse through the cell body and the dorsal root ganglia to the spinal cord. The transmission from the DRG to the spinal cord is called secondary nociception. From there, the spinal cord conveys the nociceptive signal to the brain.
Here's a cool vid showing what this process looks like in the world of computer generated animation.
http://youtu.be/PMZdkac4YLk
Modulation of nociception
Nociception can be modulated at several junctures along its pathway. This works by either facilitating or inhibiting the initiation or transmission of the nociceptive signal from one stage to the next.
When primary nociception is facilitated we call this peripheral sensitization. It is a problem "in the tissues", which usually involves chemical changes caused by inflammation. Inflammation will lower the firing threshold of nociceptors. Nociceptors can also become sensitized in the presence of adrenaline. People who have adrenally sensitive nociceptors may have increased pain that follows their hormonal state, so it may track with stress levels or menstrual cycles.
Spinal nociceptors in the area of the dorsal horn can also be sensitized so that they fire with a lower stimulus from the free nerve endings. This is called central sensitization. Moseley said that it is a mistake to consider chronic pain a disease of central sensitization. This is because central sensitization increases nociception but not necessarily pain. We know this because autopsy results from animals and humans can show significant central sensitization in subjects that did not have chronic pain.
Sensitization can also occur above the spinal cord in brain networks that process nociceptive signals. This is referred to as cortical sensitization.
Descending modulation
Nociception can also be modulated by pathways that descend from the brain. This is called descending modulation and it occurs in the dorsal horn, by facilitating or inhibiting the transmission of nociceptive impulses from the periphery to the spinal cord to the brain.
Moseley views descending modulation as a way for the brain to "second-guess" the periphery about the threat posed by a particular stimulus. For example, if the periphery is communicating information suggesting there is only a small amount of mechanical disturbance in a particular area, the brain, which has access to a wealth of additional information about what is actually going on in the periphery, may decide that the problem is far more serious, and therefore facilitate the transmission of nociceptive signals to the brain. Or the brain might use its additional information to reach the opposite conclusion and inhibit nociception. Successful manual therapies interventions probably work to some degree through descending inhibition.
Where is the sensitization?
Once we understand that nociception can be modulated at different levels, we now have more targets for intervention with a client who has chronic pain. (Instead of just focusing on the periphery where most manual therapy efforts are directed.)
For example, Moseley discussed some interesting ways to determine whether sensitization lives in the periphery (the tissues) or centrally (the dorsal horn.)
One symptom of peripheral sensitization is heat sensitivity. Therefore if heat is applied to a painful area and this does not increase the pain, it is very unlikely that the problem is a result of peripheral sensitivity mediated by inflammation. On the other hand, if heat makes the pain worse, then pain is likely the result of primary nociception.
If a peripheral area is very sensitive to mechanical inputs, but not heat, than the sensitization is likely central - at the dorsal horn. Further, cold sensitivity points in the direction of a peripheral neuropathy (disease process or injury to the nerve.)
There is of course a huge volume of other information about the physiology of nociception that was was not discussed at the conference and which I won't get into here (partly because I don't understand much of it!) One good source of information is David Butler's book the Sensitive Nervous System. It's worth a good read or three.
Cool assessment chart
Mosley made brief mention of a pain assessment chart that is available here on his website and pictured below:
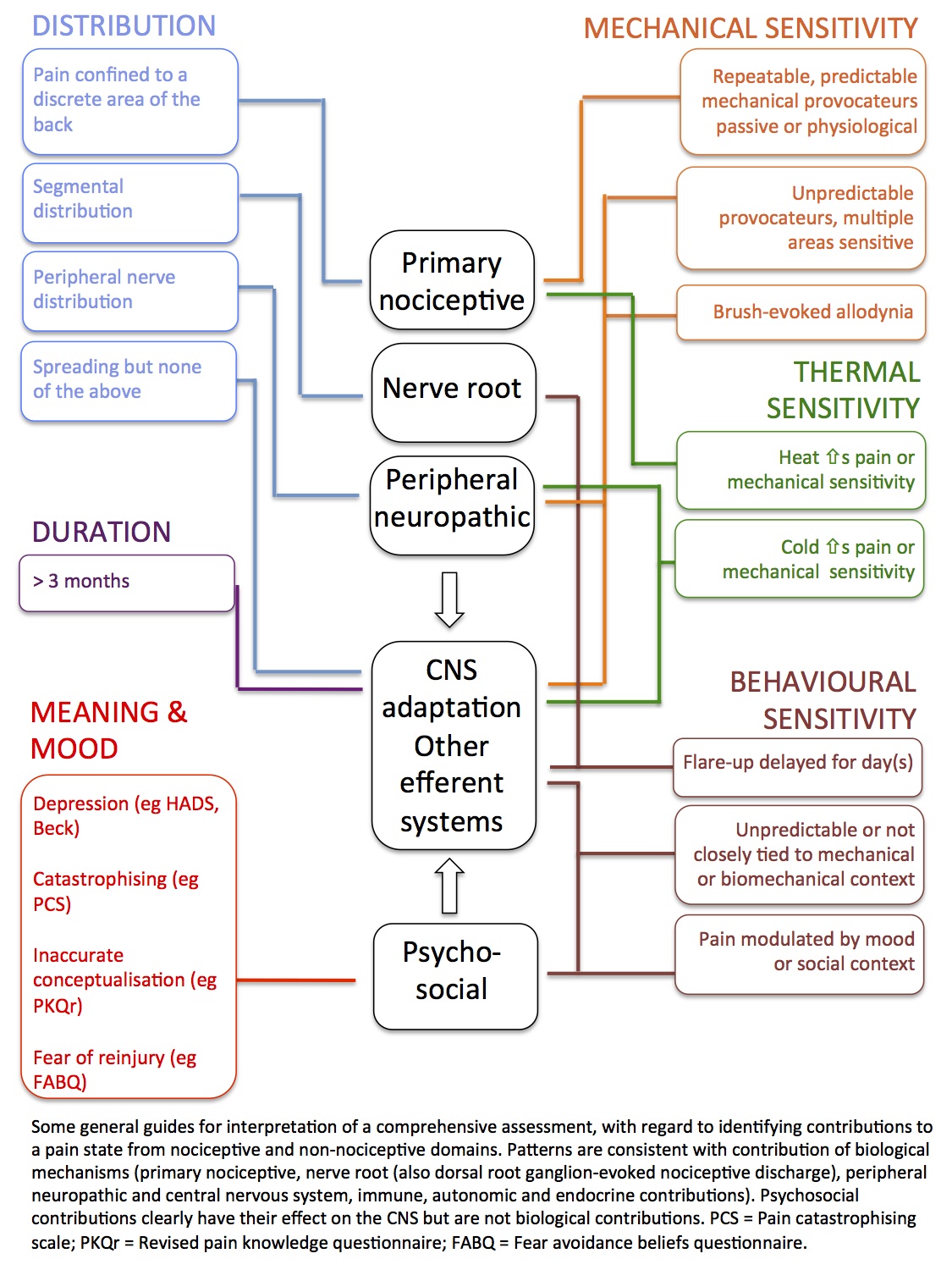
The chart tries to help a clinician understand what inputs into the system are the most imortant for creating the pain of a particular client.
For example, if the client's pain is predictably elicited by repeatable mechanical movements, then primary nociception is probably one of the key ingredients in the pain. On the other hand, if pain is rather unpredictable and brought on by a wide variety of factors, then it is likely that CNS adaptations and other outputs from the CNS are involved.
It's a cool diagram, check it out. Hopefully the type of thinking exhibited here will become more and more prominent in the way people treat clients in chronic pain.
Graded motor imagery
Lorimer also discussed his work with graded motor imagery and there is a book on the same topic which I'm going through. I've decided to make this the subject of a separate post so I won't be going into it here.
So that just about wraps this part of the review up. Thanks for reading this far! Now on to the Paul Hodges talk in the next post.
